TMJ Discomfort: Jaw Concerns You Should Know
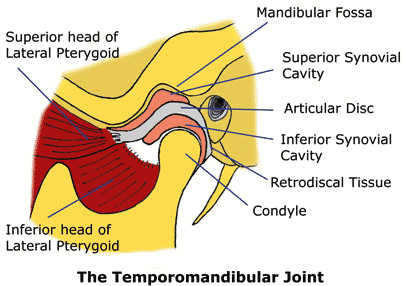
A TMJ discomfort arises when the temporomandibular joint (TMJ), which connects the jawbone to the skull, experiences dysfunction. This condition can lead to challenges in jaw movement, affecting daily activities such as speaking and chewing. Common contributing factors include joint inflammation, structural misalignments, and muscular tension. Additionally, poor posture and repetitive habits like teeth grinding can exacerbate the issue.
Temporomandibular joint (TMJ) mobility concerns may influence jaw function, postural stability, and movement efficiency. TMJ-related adaptations often involve structural and muscular influences, highlighting the need for a comprehensive, non-invasive approach to movement rehabilitation. At Chiropractic Specialty Center® (CSC), a structured model integrating chiropractic and physiotherapy methods ensures targeted jaw mobility help without reliance on invasive interventions.
Jaw function is closely linked to cervical spine movement, as postural adaptations may contribute to variations in jaw alignment. Structural changes, including articular disc displacement and muscular coordination patterns, may influence jaw movement efficiency. Extra-articular factors, such as teeth grinding, prolonged chewing, or postural strain, further impact jaw mobility. Addressing both intra-articular (joint) and extra-articular (muscular) influences ensures a well-rounded recovery approach.
CSC’s Non-Invasive Jaw & TMJ Care
Structured, non-invasive strategies focus on targeted physiotherapy techniques, manual soft-tissue mobilization, and maintaining postural alignment. High-Intensity Laser Therapy (HILT), shockwave therapy, and rehabilitative exercises assist in promoting joint flexibility and muscular coordination. Additionally, lifestyle modifications, including reducing excessive chewing and maintaining a neutral neck posture, contribute to long-term movement efficiency.
CSC’s integrative approach emphasizes spinal and jaw mobility assessments, ensuring that all movement influences are considered. By combining targeted rehabilitation techniques with structured movement strategies, individuals can work toward improved jaw function without reliance on surgical interventions. Through individualized, movement-based recovery plans, non-invasive solutions provide useful help for long-term jaw and musculoskeletal health.
Understanding the multifaceted nature of TMJ discomfort is crucial. The interplay between the jaw and cervical spine means that issues in one area can influence the other. Non-invasive approaches, such as chiropractic care, physiotherapy, and targeted rehabilitation exercises, have shown promise in addressing these concerns. By focusing on restoring proper alignment and function, individuals can work towards alleviating discomfort and improving jaw mobility.
It’s essential to consult with healthcare professionals experienced in musculoskeletal disorders to determine the most appropriate care plan. Early intervention can prevent the progression of symptoms and enhance overall quality of life.
Key Insights on TMJ Discomfort and Care
TMJ discomfort can significantly impact daily life, but understanding its causes and care options can lead to efficient management. Here are three essential points:
- Identify Contributing Factors: Recognize habits like teeth grinding, poor posture, and stress, which can strain the TMJ and surrounding muscles.
- Explore Non-Invasive Care: Chiropractic adjustments, physiotherapy, and specific exercises can address misalignments and muscle tension without surgical intervention.
- Maintain Postural Awareness: Proper neck and jaw alignment can alleviate undue stress on the TMJ. Incorporating ergonomic practices and regular movement breaks can be beneficial.
By focusing on these areas, individuals can take proactive steps toward managing TMJ discomfort and enhancing jaw function.
Experiencing TMJ Discomfort? Contact Us Today
If you’re dealing with TMJ discomfort, seeking professional guidance is crucial. Our team specializes in non-invasive approaches to address jaw function issues. Through a combination of chiropractic care, physiotherapy, and personalized rehabilitation plans, we aim to restore optimal jaw movement and alleviate discomfort.
Don’t let TMJ discomfort hinder your daily activities. Reach out to us for a comprehensive evaluation and tailored care plan. Visit our contact page to schedule an appointment and take the first step towards improved jaw health. Contact Us
Understanding TMJ-Related Discomfort and Non-Invasive Solutions
TMJ-related discomfort, commonly referred to as jaw dysfunction or ear-associated sensitivity, affects individuals experiencing jaw joint movement adaptations. This condition may contribute to jaw mobility concerns due to the connection between the temporomandibular joint (TMJ) and the surrounding musculoskeletal structures.
TMJ-related movement concerns may present with various sensations, including:
- Jaw movement sensitivity.
- Neck mobility variations.
- Generalized postural adjustments affecting jaw alignment.
Since the middle ear and TMJ are interconnected by ligaments, jaw-related adaptations may occasionally influence ear sensitivity and movement comfort.
At Chiropractic Specialty Center® (CSC), our structured, movement-based approach integrates chiropractic and physiotherapy rehabilitation methods to maintain TMJ function and postural efficiency.
Common Factors Contributing to TMJ-Related Discomfort
TMJ function changes may arise due to various structural and postural adaptations. Identifying the underlying influences is key to a well-structured movement recovery strategy.
Primary Contributing Factors:
- Joint Inflammation – TMJ movement sensitivity may result from joint swelling affecting mobility.
- Structural Adjustments – Variations within jaw joint alignment may influence movement patterns.
- Movement Efficiency Changes – Wear and tear in the jaw joint structure may impact jaw mobility.
- Postural Influences – Cervical spine alignment adjustments may contribute to jaw movement adaptations.
While intra-articular factors (joint-related concerns) may contribute to TMJ-related movement patterns, extra-articular influences (muscular and postural factors) may also affect jaw mobility and flexibility.
The Influence of Cervical Spine Movement on TMJ Function
The neck and jaw joint function are closely interconnected, with cervical movement adaptations potentially contributing to jaw mobility variations.
- Upper cervical spine movement patterns may influence jaw positioning and alignment.
- Repetitive jaw muscle activity, such as prolonged chewing or teeth grinding, may contribute to jaw joint strain.
Addressing both intra-articular (joint) and extra-articular (muscular) movement influences ensures a comprehensive approach to TMJ movement help.
Targeted, Non-Invasive Solutions for TMJ Movement Care at CSC
At CSC, we integrate structured, movement-based CSC’s nearby physiotherapyin KL and chiropractic care by reigstered chiros in Kuala Lumpur methods to provide a non-invasive approach to TMJ function rehabilitation.
Our collaborative clinical model ensures that movement strategies align with both muscular coordination and joint mobility needs. By combining targeted rehabilitation methods with individualized care strategies, we offer a structured, movement-based approach to jaw mobility and flexibility care.
Intra-Articular Considerations in Jaw Joint Movement
Intra-articular influences involve changes within the jaw joint structure, which may contribute to TMJ-related mobility concerns. Identifying joint function variations ensures a structured movement recovery plan to help long-term jaw mobility and postural alignment.
Primary Joint Considerations:
- Inflammation affecting jaw joint mobility.
- Structural movement adaptations influencing TMJ flexibility.
- Postural alignment concerns contributing to jaw movement limitations.
Targeted Care for Jaw Joint Mobility:
- Synovitis (Joint Synovium Sensitivity):
- Involves movement sensitivity due to inflammation in the jaw joint’s synovial tissue.
- May contribute to jaw stiffness and mobility variations.
- Internal Structural Adjustments:
- Jaw function changes due to direct or indirect movement adaptations.
- Common influences include repetitive chewing, teeth grinding, or postural misalignments.
Variations in Jaw Joint Disc Movement
Structural changes within the jaw joint disc may contribute to movement efficiency adaptations. The jaw joint disc plays a role in cushioning movement, ensuring that jaw mobility remains efficient.
Types of Jaw Joint Disc Variations:
- Disc Displacement with Reduction:
- The articular disc shifts from its original position but returns during movement.
- May be associated with jaw clicking or movement variations.
- Disc Displacement without Reduction:
- The articular disc remains displaced, contributing to joint movement limitations.
- May result in jaw mobility restrictions and postural adaptations.
A Structured Approach to Jaw Mobility Care
At CSC, our non-invasive rehabilitation strategies provide a movement-based recovery model for individuals experiencing jaw movement concerns.
By integrating structured movement rehabilitation, physiotherapy, and chiropractic techniques, we ensure that TMJ function is supported through a targeted, movement-based recovery model.
Understanding Articular Disc Displacement and Jaw Mobility Adaptations
Articular disc displacement may contribute to jaw movement variations, sometimes influencing ear sensitivity due to the structural connections between the jaw and surrounding musculoskeletal tissues.
Individuals experiencing articular disc displacement without reduction may notice:
- Jaw movement deviations toward the affected side.
- Variations in jaw mobility without an audible clicking sound.
- Occasional jaw locking, sometimes accompanied by movement-related sounds.
When the articular disc shifts from its original position, the supportive tissues of the jaw joint may experience strain, leading to changes in mobility efficiency. The disc may shift medially or laterally, potentially producing movement-related sensations, such as a mild popping sound.
In early stages, there may be minimal to no movement sensitivity, but as displacement progresses, individuals may experience variations in jaw function.
Arthritis and Jaw Joint Function
Arthritic movement adaptations may influence jaw mobility and structural alignment, contributing to jaw function variations. Two primary forms of arthritis that may influence jaw movement efficiency include:
- Degenerative Movement Adaptations:
- More commonly associated with long-term jaw mobility variations.
- Structural movement changes may include flattening of the condylar head or bone surface variations.
- Often observed in individuals over 50, though younger individuals with previous jaw movement concerns may also experience similar changes.
- Inflammatory Joint Adaptations:
- May occur in conditions such as rheumatoid arthritis, ankylosing spondylitis, or gout.
- Often accompanied by movement sensitivity, swelling, or changes in jaw mobility efficiency.
Early intervention with structured, movement-based strategies may help maintain jaw mobility and musculoskeletal function before these conditions progress further.
Extra-Articular Influences on Jaw Mobility and Comfort
Jaw mobility variations may also be influenced by extra-articular factors, including muscular coordination patterns, postural movement efficiency, and connective tissue function.
Common extra-articular influences include:
- Jaw muscle movement patterns.
- Neck and postural adaptations.
- Tendon function changes.
- Previous jaw-related structural concerns.
A comprehensive, movement-based recovery approach involves assessing both intra-articular and extra-articular factors to ensure that all structural and muscular influences are considered.
Jaw Muscle Adaptations and Mobility Care
Muscular function plays an essential role in jaw mobility and coordination. Trismus, or muscle tension affecting jaw movement, may contribute to limited jaw mobility efficiency.
The primary jaw movement muscles include:
- Masseter muscle – Maintain jaw closure and chewing efficiency.
- Temporalis muscle – Assists in jaw movement stabilization.
- Pterygoid muscles – Play a role in jaw positioning and alignment.
Muscle coordination changes may arise due to:
- Stress-related muscle tension.
- Jaw movement patterns involving excessive chewing or teeth grinding.
- Postural adaptations influencing muscular coordination.
Postural Adaptations and Jaw Function
Neck movement efficiency is closely linked to jaw positioning and mobility patterns. The anterior belly of the digastric muscle, which connects the jaw to the hyoid bone, plays a key role in jaw movement coordination.
Forward head posture and extended neck positioning may contribute to:
- Excessive jaw movement pressure.
- Structural misalignment affecting joint function.
- Variations in jaw movement efficiency over time.
Minimizing prolonged forward head movement, such as extended screen time or repetitive forward-leaning positions, may assist in jaw mobility efficiency and postural stability.
Temporal Tendon Considerations in Jaw Function
Temporal tendinopathy involves muscular and connective tissue adaptations in the temporalis region, sometimes influenced by jaw function patterns such as teeth grinding or excessive jaw movement repetition.
Individuals with temporal tendinopathy may experience:
- Movement sensitivity in the temporal region of the skull.
- Variations in jaw movement efficiency.
- Occasional postural strain affects jaw coordination.
Jaw Structural Concerns and Their Influence on Mobility
Jaw structural changes, including fractures or previous movement concerns, may contribute to jaw mobility efficiency variations.
- Mandibular fractures – Often associated with structural movement adaptations following jaw trauma.
- Condylar neck variations – May influence jaw mobility and movement alignment.
Spinal and Jaw Movement Efficiency
Spinal mobility plays a role in jaw function and postural coordination. Research suggests that approximately 70% of individuals experiencing jaw movement variations may also have cervical spinal function adaptations.
At CSC, we integrate spinal mobility assessments for individuals experiencing jaw movement concerns. Our structured approach ensures that both spinal and jaw function assessments are considered in movement-based rehabilitation strategies.
Studies, such as research published by Dr. Ciancaglini, Dr. Testa, and Dr. Radaelli in the Scandinavian Journal of Rehabilitation Medicine (1999), highlight the connection between cervical spinal movement adaptations and jaw mobility efficiency.
By integrating spinal function assessments into jaw movement recovery models, CSC ensures a structured, movement-based approach to jaw mobility rehabilitation.
Additional Factors Contributing to Jaw Mobility Concerns
Various conditions may influence jaw mobility and function, contributing to movement adaptations and muscular coordination changes. Understanding the underlying influences allows for a structured, movement-based approach to jaw mobility care.
Common Influences on Jaw Function:
- Pseudo-hypomobilities – Includes muscular adaptations, previous jaw procedures, soft-tissue sensitivities, postural influences, and structural movement adjustments.
- True hypomobilities – May involve long-term post-surgical movement adaptations, joint mobility concerns, and connective tissue flexibility variations.
Understanding these potential influences allows for a structured, movement-based rehabilitation model that helps jaw function and postural efficiency.
While general insights may provide helpful guidance, self-diagnosis and self-care approaches should be avoided. For structured movement rehabilitation, individuals are encouraged to consult qualified professionals specializing in musculoskeletal movement function.
At Chiropractic Specialty Center® (CSC), our chiropractors and physiotherapists provide a structured movement-based approach, ensuring that jaw mobility and musculoskeletal function are supported through individualized movement strategies.
Lifestyle Recommendations for Maintaining Jaw Mobility
Simple lifestyle adjustments may assist in reducing excessive jaw strain and maintaining movement efficiency.
Jaw Function Care Strategies:
- Consume softer foods such as pasta and soups to minimize jaw movement strain.
- Modify food texture by cutting meals into smaller portions to avoid excessive chewing pressure.
- Maintain a neutral neck posture and minimize prolonged head bending.
- Avoid prolonged chewing activities, including chewing gum, which may contribute to jaw muscle strain.
- Reduce consumption of harder foods, such as raw vegetables, nuts, and hard candies.
- Minimize excessive jaw movements, such as crunching ice or opening the mouth widely when yawning.
- Limit caffeine intake, as it may influence muscular tension.
- Consider nutritional care, such as Vitamin C and magnesium, to encourage muscle coordination and recovery.
- Alternate heat and cool applications by applying moist heat for five minutes, followed by a five-minute cool massage on the jaw area.
- Practice gentle muscle relaxation techniques, such as light temporal area massage, for five to ten minutes.
If jaw mobility variations persist, structured movement-based rehabilitation may be necessary. At CSC, our team of chiropractors and physiotherapists provides individualized movement rehabilitation strategies tailored to jaw function and postural stability.
Targeted Movement Rehabilitation for Jaw Function in Malaysia
For long-term jaw function care, a structured movement rehabilitation strategy is essential. Many individuals experiencing jaw movement concerns may also have cervical spinal function variations, emphasizing the importance of an integrative movement-based recovery approach.
At CSC, our team specializes in jaw function rehabilitation, integrating:
- Targeted chiropractic techniques to maintain jaw and cervical spinal alignment.
- Movement-based physiotherapy strategies designed to encourage jaw mobility and muscle coordination.
- Collaborative care models, including referrals to dental professionals when needed, ensuring a comprehensive recovery approach.
Over the past 15 years, CSC has supported numerous individuals experiencing jaw function adaptations, ensuring that both jaw mobility and postural movement influences are addressed through structured rehabilitation techniques.
For structured, non-invasive care from specialists in jaw movement rehabilitation, contact CSC today to receive an individualized movement-based recovery plan.
Author:
“TMJ Discomfort: Jaw Concerns You Should Know” is written by Yama Zafer, D.C., with an educational background in physiotherapy and chiropractic from Cleveland Chiropractic University in Kansas City, has dedicated nearly three decades to the fields of physiotherapy and chiropractic care. Read more about Y. Zafer.
Peer-Reviewed Medical References:
- Alowaimer, A. N., et al. (2024). Comparative Efficacy of Non-Invasive Therapies in Temporomandibular Joint Dysfunction: A Systematic Review. Journal of Oral Rehabilitation.
- Abouelhuda, A. M., et al. (2018). Non-invasive different modalities of treatment for temporomandibular disorders: review of literature. Journal of Korean Association of Oral and Maxillofacial Surgeons, 44(2), 43–51.
- WebMD. (n.d.). TMJ Disorder: Causes, Symptoms, and Treatment.
- StatPearls. (n.d.). Temporomandibular Syndrome. NCBI Bookshelf.
- Verywell Health. (n.d.). Physical Therapy for Temporomandibular Joint Dysfunction (TMJ).
- The Guardian. (2024). Does your jaw click? Do you grind your teeth? It could be this little-known condition.
- Healthdirect Australia. (n.d.). Temporomandibular joint dysfunction – symptoms, treatment and causes.
Last Updated:
Last updated on August 19, 2025: TMJ Discomfort: Jaw Concerns You Should Know.
