Comprehensive Non-Surgical Support for Spondylolisthesis
This article provides an in-depth look at spondylolisthesis, a condition where one vertebra shifts forward over the one below it, affecting spinal stability and mobility. It explores the causes, symptoms, and differences between spondylolisthesis, spondylosis, and spondylolysis, helping individuals understand the distinctions between these spinal conditions.
Early identification and lifestyle adjustments play a crucial role in managing spondylolisthesis, as symptoms may range from mild stiffness to nerve-related sensations in the legs. The article highlights the importance of MRI and X-ray imaging in assessing vertebral slippage, nerve involvement, and spinal function, ensuring accurate evaluation and informed care strategies.
Non-surgical management options include chiropractic techniques, physiotherapy-based rehabilitation, spinal decompression (RxDecom®), NSD Therapy®, and guided spinal stabilization exercises. These approaches focus on improving spinal alignment, reducing nerve compression, and enhancing overall mobility. The article also emphasizes preventive strategies, such as maintaining proper posture, engaging in low-impact exercises, and using ergonomic support to reduce spinal strain and prevent progression.
For those experiencing spondylolisthesis-related mobility concerns, Chiropractic Specialty Center® (CSC) offers personalized, non-surgical spinal care, integrating advanced technology and evidence-based rehabilitation methods. The article encourages early intervention and structured spinal care to improve long-term spinal function and quality of life.
Understanding Spondylolisthesis
Spondylolisthesis occurs when one vertebra shifts forward over the one below it (slipped vertebra), affecting the spine’s alignment. This condition often results from factors such as age-related wear, congenital abnormalities, or injuries to the spine. While spondylolisthesis can impact mobility, its severity varies depending on the extent of the vertebral shift.
The shifting, vertebral misalignment, and slipping forward of a vertebra over the one beneath may lead to spinal instability. The slippage in spondylolisthesis can result from congenital defects, degenerative changes, or traumatic injuries. Recognizing early signs, such as lower back discomfort or stiffness, is essential for prompt management and preventing progression.
Early identification is essential to managing the condition effectively and maintaining quality of life. Individuals experiencing reduced flexibility or a sensation of tightness in the lower back may find it helpful to explore available non-invasive approaches to support spine health.
Signs and Symptoms of Spondylolisthesis
Spondylolisthesis can present a variety of signs and symptoms depending on the severity of the condition and the degree of vertebral misalignment. In mild cases, individuals may not notice any significant symptoms. However, as the condition progresses, noticeable physical changes and discomfort can arise.
One common sign is a reduced range of motion in the lower back, making it difficult to bend or twist. This stiffness may be accompanied by tightness in the surrounding muscles, particularly in the hamstrings. Some individuals report a sensation of instability in their lower back, which can affect daily activities like walking or standing for extended periods.
In certain cases, nerve compression from the shifted vertebra may lead to radiating sensations along the legs. This condition, often referred to as sciatica-like discomfort, may include tingling, numbness, or a pins-and-needles sensation in the thighs or calves. Postural changes, such as a visible curvature or a forward-leaning stance, are also possible.
Recognizing these symptoms early is essential for effective management. Addressing lifestyle changes, such as engaging in gentle exercises and adopting better ergonomic practices, can support spinal stability. If you experience any of these signs, consult a qualified healthcare provider to explore non-invasive approaches for promoting spinal health.
Understanding the Differences: Spondylolisthesis, Spondylosis, and Spondylolysis
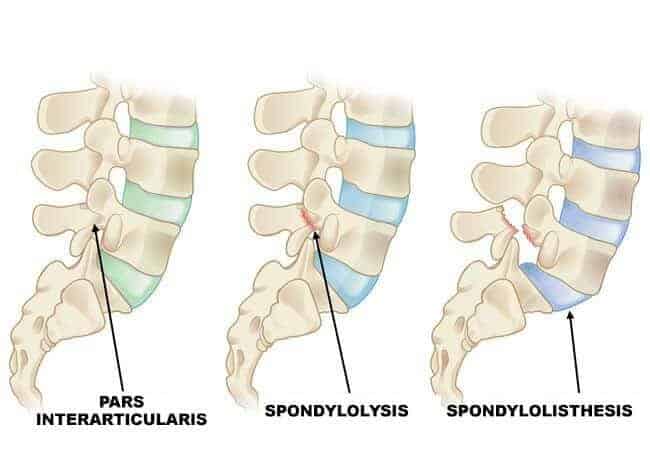
Spondylolisthesis, spondylosis, and spondylolysis are spinal conditions with distinct characteristics, though their similar names often cause confusion. Understanding their differences can help individuals better recognize and address spinal health concerns.
- Spondylolisthesis involves the forward displacement of one vertebra over another. This condition typically arises due to stress fractures in the vertebral structure, congenital abnormalities, or degeneration from aging. Spondylolisthesis often affects the lower back, leading to changes in mobility or pressure on nearby nerves.
- Spondylosis, on the other hand, refers to general wear-and-tear changes in the spine due to aging. These degenerative changes may include disc thinning, bone spurs, or joint stiffness. Unlike spondylolisthesis, spondylosis is a more widespread condition affecting the overall structure of the spine rather than causing vertebral displacement. Spondylosis may result in stiffness or reduced spinal flexibility, especially in the neck or lower back.
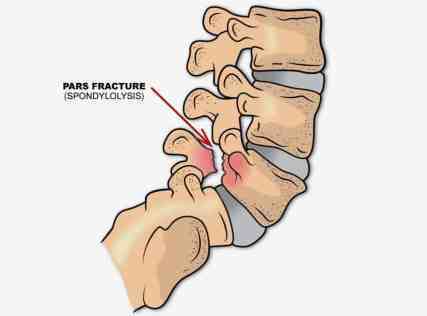
- Spondylolysis is a specific defect or fracture in a part of the vertebra called the pars interarticularis. This condition often affects younger individuals, particularly athletes engaged in repetitive hyperextension activities. Spondylolysis can lead to spondylolisthesis if the defect progresses, but not all cases develop into vertebral slippage.
In summary, spondylolisthesis is vertebral slippage, spondylosis is age-related spinal degeneration, and spondylolysis is a structural defect in the vertebra. Recognizing these distinctions is crucial for addressing the specific needs of each condition through tailored approaches for spinal health and well-being.
The Role of MRI and X-Rays in Evaluating Spondylolisthesis
Accurate identification and assessment of spondylolisthesis require advanced imaging techniques, with MRI and X-rays serving complementary roles. Both tools are critical in identifying the underlying causes and evaluating the severity of the condition, enabling informed clinical decisions.
Magnetic Resonance Imaging (MRI) is essential for visualizing soft tissues, such as spinal discs, ligaments, and nerve roots. MRI scans provide detailed images of the ligamentum flavum, intervertebral discs, and any evidence of nerve compression or encroachment. This level of detail is vital for understanding how spondylolisthesis impacts the spinal nerves and surrounding structures, which may contribute to discomfort or altered mobility.
A study published in the Journal of Clinical Imaging Science highlights MRI as the gold standard for assessing nerve involvement and detecting degenerative changes associated with spondylolisthesis.
X-rays, on the other hand, are indispensable for evaluating the bony structure and stability of the spine. Standard lateral X-rays show the degree of vertebral slippage, while specialized lateral flexion and extension views assess spinal stability during movement. These dynamic images help determine whether the condition is stable or worsening, aiding in decisions about non-invasive care or further interventions.
Together, MRI and X-rays offer a comprehensive picture of spondylolisthesis, ensuring a thorough understanding of spinal health and guiding individualized care plans.
For an in-depth study on the utility of imaging in spinal conditions, see the findings in the European Spine Journal, which underscore the complementary roles of these tools in spinal assessments.
Prioritizing Lifestyle Changes for Spine Health
Adopting a spine-friendly lifestyle plays a crucial role in managing spondylolisthesis. Regular, low-impact exercises like walking or swimming can enhance mobility and support the spine. Maintaining a balanced diet rich in nutrients ensures better spinal health, particularly for vertebrae and supporting muscles.
Using ergonomic furniture and practicing proper lifting techniques help reduce stress on the back. Being mindful of daily habits can improve spine support over time. For those seeking professional insights, consulting healthcare practitioners about options aligned with specific conditions is encouraged.
What Causes Spondylolisthesis?
Spondylolisthesis can result from congenital conditions, traumatic injuries, or degenerative changes in the spine.
Common Causes
- Congenital Factors:
Birth-related structural abnormalities in the spine are a primary cause of spondylolisthesis. - Traumatic Injuries:
Events such as slips, falls, or automobile accidents can lead to fractures or damage that cause forward slippage of the vertebra. This type of injury-related spondylolisthesis is often linked to spondylolysis, a specific spinal defect discussed below. - Degenerative Changes:
Premature wear and tear in the spine often result from conditions like:- Degenerative Disc Disease (DDD): Dehydration and degeneration of spinal discs.
- Spinal Arthritis: Excessive arthritic changes in the spinal joints, also known as facet hypertrophy.
- Ligament Damage: Issues with ligaments such as the ligamentum flavum, which can lead to instability.
What Is Spondylolysis?
Spondylolysis refers to a defect or fracture in the pars interarticularis, a small bony projection in the back of the spinal vertebra. This condition can result from injuries or degenerative changes over time.
Types of Spondylolysis
- Traumatic Spondylolysis:
Sudden injuries such as falls, car accidents, or sports activities can cause fractures in the pars interarticularis, leading to spondylolysis. - Degenerative Spondylolysis:
Common in older adults, this form develops gradually due to bone-weakening conditions like osteoporosis or osteopenia. These conditions increase the risk of fractures in the pars interarticularis.
Spondylolysis and Spondylolisthesis
Spondylolysis often leads to forward slippage of a vertebra, resulting in spondylolisthesis. When both conditions are present, the diagnostic term used is spondylolysis with spondylolisthesis. The severity of forward slippage is categorized into grades, depending on the extent of displacement.
Understanding Spondylolysis and Its Relationship to Spondylolisthesis
Bone-Weakening Conditions and Spondylolysis
The primary factor in developmental spondylolysis is a bone-weakening condition, such as osteoporosis or osteopenia. Patients with reduced bone mineral density are at a higher risk of developing cracks or fractures in the spine, particularly in the pars interarticularis.
- Pars Interarticularis: A small bony structure located in the back of the vertebrae, forming part of the spinal joints.
- Stress Accumulation: In weakened bones, cumulative stress can lead to breaks or cracks in the pars interarticularis, progressing to fractures.
Individuals with advanced degenerative spine conditions, including osteoporosis, are at an increased risk of developing spondylolysis due to the compromised strength of the vertebrae.
Spondylolysis and Forward Slippage (Spondylolisthesis)
Spondylolysis is characterized by defects or fractures in the pars interarticularis. This condition often presents with forward slippage of the vertebra, a hallmark of spondylolisthesis.
- When spondylolysis is accompanied by forward slippage, the condition is referred to as spondylolysis with spondylolisthesis.
- The severity of forward slippage in spondylolisthesis is graded based on the extent of displacement, with higher grades indicating more significant slippage.
What Are the Categories of Spondylolisthesis?
Spondylolisthesis refers to the forward slippage of one vertebra over the one below it. This condition is graded based on the percentage of slippage, regardless of whether it occurs due to a defect in the pars interarticularis or other spinal instabilities.
Grading Scale for Spondylolisthesis
- Grade I: Slippage of less than 25%.
- Grade II: Slippage between 26% and 49%.
- Grade III: Slippage between 50% and 74%.
- Grade IV: Slippage of 75% or more.
What Are the Different Grades of Spondylolisthesis?
Spondylolisthesis is categorized into four grades based on the degree of forward slippage of one vertebra over the one below it. This grading system helps healthcare providers determine the severity of the condition and guide appropriate management strategies.
- Grade I (Slippage less than 25%)
This is the mildest form of spondylolisthesis. Many individuals with Grade I slippage experience little to no symptoms and can often maintain their regular activities with minimal disruption. Management typically includes lifestyle modifications, such as maintaining proper posture and incorporating gentle exercises to strengthen core and spinal muscles. - Grade II (Slippage between 26% and 49%)
Symptoms may become more noticeable at this stage, including lower back discomfort, reduced range of motion, and muscle tightness. Non-invasive care like physiotherapy, chiropractic techniques, and ergonomic adjustments are commonly recommended. These interventions aim to stabilize the spine and prevent further slippage. - Grade III (Slippage between 50% and 74%)
This moderate level of slippage often causes more pronounced symptoms, such as radiating sensations along the legs (sciatica-like discomfort) or visible postural changes. A comprehensive care plan, including advanced therapeutic approaches like spinal decompression or customized exercise programs, can help manage the condition without surgery. - Grade IV (Slippage of 75% or more)
This is the most severe form, typically associated with significant spinal instability and more severe symptoms. While surgical intervention may be considered for advanced cases, a non-invasive approach using targeted therapies is often recommended as an initial step, particularly for individuals seeking alternatives to surgery.
Understanding the grade of spondylolisthesis helps ensure that care is tailored to the specific needs of the individual, supporting both spinal stability and overall quality of life.
How Is Spondylolisthesis Managed Without Surgery?
Non-surgical management of spondylolisthesis focuses on enhancing spinal stability, mobility, and overall function. This approach combines evidence-based techniques, lifestyle modifications, and professional care to provide comprehensive support.
- Low-Impact Exercises
Activities such as walking, swimming, or yoga can strengthen the muscles supporting the spine without placing undue stress on the affected area. Core-strengthening exercises, particularly those targeting the abdominal and back muscles, are critical for improving spinal stability. - Ergonomic Adjustments
Making changes to daily habits, such as using ergonomic chairs or standing desks, reduces strain on the lower back. Proper posture during sitting, standing, and lifting activities is crucial for maintaining spinal alignment. - Physiotherapy
Guided physiotherapy sessions focus on strengthening the muscles around the spine and improving flexibility. Techniques such as manual therapy, stretching, and balance exercises are customized to the individual’s needs. - Chiropractic Care
Gentle, targeted chiropractic methods can help improve spinal alignment and support overall spinal health. Chiropractors use non-invasive techniques to reduce strain on the affected vertebra and enhance mobility. - NSD Therapy®: NSD Therapy® is a unique system of non-surgical spine care that utilized spinal decompression therapy, physiotherapy with non-rotatory chiropractic care as primary method in managing patients with spondylolisthesis.
- Lifestyle Changes
Maintaining a healthy weight reduces pressure on the spine. Adopting a balanced diet rich in nutrients supports bone health, while quitting smoking can improve circulation and tissue repair.
This integrated approach not only addresses current symptoms but also prevents the condition from worsening, helping individuals maintain an active and fulfilling lifestyle.
Can Spondylolisthesis Be Prevented?
While not all cases of spondylolisthesis are preventable, taking proactive steps to protect spinal health can significantly reduce the risk. Here are some strategies to minimize the likelihood of developing or worsening this condition:
- Maintain a Healthy Weight
Excess weight places additional strain on the spine, increasing the risk of vertebral slippage. A balanced diet rich in calcium, vitamin D, and other nutrients supports bone strength and overall spinal health. - Practice Good Posture
Standing and sitting with proper alignment minimizes stress on the lower back. Avoid slouching or prolonged periods of sitting, and consider ergonomic furniture to support natural spinal curves. - Engage in Low-Impact Exercises
Activities like swimming, walking, or cycling strengthen the muscles that support the spine without causing excessive stress. Core-strengthening exercises are particularly beneficial for improving stability. - Avoid Repetitive Back Strain
Athletes and individuals involved in repetitive motions, such as lifting or bending, should use proper techniques to reduce strain. Wearing supportive gear and taking breaks during strenuous activities can also help. - Early Intervention for Spinal Concerns
If you experience lower back tightness, reduced flexibility, or other early signs of spinal instability, seek professional guidance. Addressing issues promptly can prevent further degeneration or vertebral slippage.
By adopting these spine-friendly habits, individuals can enhance spinal health and reduce the likelihood of developing conditions like spondylolisthesis. These preventative measures also contribute to overall well-being, allowing for a more active and comfortable lifestyle.
Managing Spondylolisthesis Based on Grade
- Grade I and II: These are generally managed non-surgically through targeted chiropractic care and physiotherapy. At CSC, we offer integrative care tailored to stabilize the spine and improve overall function.
- Grade III and IV: Surgical intervention may be considered, especially for severe cases. However, factors such as patient age and overall health should be carefully evaluated to determine the best course of action.
Spondylolysis vs. Spondylolisthesis
- Spondylolysis: Refers to a defect or fracture in the pars interarticularis without forward slippage.
- Spondylolysis with Spondylolisthesis: Occurs when slippage accompanies the defect. This condition may be congenital (present at birth) or develop later due to an acute injury or degenerative changes.
Spondylolisthesis Management
Spondylolisthesis, involving the forward slippage of one vertebra over another, can often worsen without proper care. Early management is critical to support spinal health and prevent complications. Non-invasive approaches that focus on improving spinal stability and addressing associated soft tissue issues are often recommended.
CSC combines targeted care with a focus on improving stability, alignment, and function. Our team works to ensure each approach is safe, precise, and tailored to the individual’s condition.
A CSC Care Approaches
To complement manual techniques, advanced therapy methods are used to support the recovery process. These include:
- Spinal Decompression Therapy to reduce pressure on discs.
- Muscle-Specific Strengthening to improve support and stability.
- Soft Tissue Focused Techniques for addressing imbalances and promoting recovery.
- NSD Therapy® Protocols Specific for Spondylolisthesis: Non-invasive care by physios and chiros of CSC
Supporting Overall Spinal Health
Conditions like spondylolisthesis often coincide with other spinal concerns, such as:
- Joint and disc-related changes.
- Muscular imbalances.
- Changes in posture or alignment.
Comprehensive care ensures that these related issues are managed to promote overall recovery and spinal health.
Top 7 FAQs on Spondylolisthesis
Answer:
Spondylolisthesis is a spinal condition where one vertebra slips forward over the one beneath it. This condition can result from congenital abnormalities, stress fractures, degenerative changes, or traumatic injuries. It is commonly seen in the lower back (lumbar spine) and may cause issues with spinal stability. Early identification and understanding the cause of spondylolisthesis are essential for proper management and improving mobility.
Answer:
Symptoms vary depending on the severity of the vertebral slippage. Mild cases may present no noticeable signs, while moderate to severe cases can include reduced flexibility, tightness in the lower back, or sensations like tingling and numbness in the legs. Some individuals also report posture changes, difficulty standing for long periods, or sciatica-like discomfort, which includes radiating sensations along the legs.
Answer:
Diagnosis involves a combination of clinical evaluation and imaging techniques. X-rays are used to assess vertebral alignment and spinal stability during motion (e.g., flexion and extension views). MRI is considered the gold standard for evaluating soft tissues, such as discs, nerves, and ligaments, and identifying nerve involvement or degenerative changes. These tools provide a comprehensive understanding of the condition.
Answer:
Spondylolisthesis is classified into grades based on the percentage of vertebral slippage:
Grade I: Slippage less than 25%.
Grade II: Slippage between 26% and 49%.
Grade III: Slippage between 50% and 74%.
Grade IV: Slippage of 75% or more.
Grades I and II are often managed non-invasively, while Grades III and IV may require more advanced interventions.
Answer:
Non-surgical management focuses on improving spinal stability and reducing discomfort. Common approaches include low-impact exercises, ergonomic modifications, physiotherapy for strengthening supportive muscles, and chiropractic care for improved spinal alignment. A tailored care plan helps slow progression and maintain mobility. Lifestyle changes, such as weight management and posture correction, further support spinal health.
Answer:
Spondylolisthesis: Forward slippage of a vertebra over the one below it, caused by defects, degeneration, or trauma.Spondylolysis: A fracture or defect in the pars interarticularis of a vertebra, which may lead to spondylolisthesis.Spondylosis: General age-related degeneration of the spine, leading to issues like disc thinning and bone spurs but without vertebral slippage.Recognizing these distinctions is essential for choosing the right care plan.
Answer:
While not all cases can be prevented, certain lifestyle choices can reduce the risk. Maintaining a healthy weight, practicing good posture, and engaging in regular, low-impact exercises strengthen the spine and surrounding muscles. Avoiding repetitive stress or strain on the lower back, especially in sports, can also help. Early intervention for spinal health concerns can further mitigate risks.
Content Coverage: Not explicitly covered. This topic should be added for completeness.


Cervical spondylosis
Dear Deedy,
Our centers offer the best non-invasive treatment for cervical spondylosis. We have emailed you and hope to hear from you soon.
Hello, my mum was diagnosed with spondylolisthesis here in Nigeria. What kind of suggestions will you offer on how to treat her, please.
Dear Bawa,
Spondylolisthesis is a condition best managed through our methods of physical therapy (physiotherapy) and chiropractic in Malaysia. But, per your comment, your mother lives in Nigeria. So, my best advice is to a non-surgical center capable of providing her the care she needs. Surgery is an option for unstable spondylolisthesis.
Unstable spondylolisthesis is a condition that progressively worsens with time. In other words, they progress from a Grade-I to a Grade-II, and so forth. So, if the slippage of the vertebrae has progressed, she may be a candidate for surgery. In our centers, we have devices and technology that can stabilize an unstable spondylolisthesis in some patients. If you wish to get care from our center, please contact our main physical therapy and chiropractic center here in Kuala Lumpur Malaysia. You call our center at +(60)3 2093 1000.
I hope this information was helpful.
Hi, I have spondylolisthesis at level two, but my leg is weak and in severe pain. The doctor is saying that maybe they will do surgery on my back. So do you have any suggestions? Thanks
Dear Harpreet,
Spondylolisthesis is treatable and manageable without surgery. My recommendation to anyone with back pain resulting from spinal disc herniation, arthritis, or spondylolisthesis is to exhaust an effective conservative approach before contemplating a surgical intervention.
I do so because surgery for spondylolisthesis requires screws and rods. According to published medical reports, 74% of spinal fusion surgery patients will have to live with some degree of pain after surgery. In short, if you were to get your surgery in the US, you would have to live with some degree of pain or disability. Therefore, it would be better to get a spondylolisthesis-specific therapy and treatment programs that eliminate your pain without the risks of surgery or the possibility of post-surgical back pain.
What is the best treatment for spondylolisthesis?
The best treatment for spondylolisthesis is a non-surgical route that combines a non-rotatory system of chiropractic, physiotherapy, and rehabilitation. NSD Therapy® service is the best option. In Malaysia, we are the only NSD Therapy® providers. We have successfully treated many with spondylolisthesis and those with post-surgical pain. Contact our main center today for locations or more information on the type of care we provide; please WhatsApp our main center. At CSC, you get the best chiropractic combined with physiotherapy; visit or call us today. I hope this helped.
I have severe back pain with footdrop. Been a couple months. Need help, thanks….
Dear Phillip,
Please accept our sincere apology for not responding sooner.
Since you didn’t provide an MRI report or specific findings, I’ll base my response on common causes associated with these symptoms, particularly as you’ve posted this query in the spondylolisthesis section. Also, please keep in mind that the information I provide in any reply is meant to give you information, and it does not replace or substitute for a consultation or recommendation for management, as I have not assessed you.
At CSC, we specialize in conservative treatments that have successfully managed conditions similar to yours. Our integrative therapy approach, which incorporates chiropractic care, physiotherapy, spinal decompression, and focused rehabilitation, has shown positive outcomes for many patients experiencing back pain and neurological symptoms like foot drop.
Foot drop typically occurs when there is nerve damage or compression at certain points along the nerve pathway that controls the muscles involved in lifting the foot. This can result from spinal issues such as canal stenosis, where narrowing of the spinal canal compresses the nerves that travel to the lower limbs.
While I regret that the limited information provided restricts more detailed advice, I strongly encourage you not to let this deter you from seeking further help. It’s crucial to have a thorough evaluation, which might include an MRI, to better understand the specific causes of your symptoms. An accurate diagnosis will allow for a tailored treatment plan that addresses your specific needs. However, I will try my best to give you some information on conditions commonly known to cause foot drop and what you can do to feel better without surgery.
Common conditions that cause canal stenosis and foot drop include:
• Spondylolisthesis: This is a forward slippage of vertebrae in relation to the segment Spondylolisthesis is a condition where the vertebrae slip forward in relation to the segment below. The severity of this condition is rated from grade 1 to 4. Grade 1 usually does not cause foot drop unless it is unstable or there is a bulging or herniated disc. However, grade 2 and higher can result in foot drop since they are always unstable.
• Herniated or bulging discs: Also known as slipped discs, can also lead to foot drop if the bulge or herniation is moderate or more severe.
• Thickening of ligamentum flavum (yellow ligament): Hypertrophy of the ligamentum flavum is a relatively common cause of canal stenosis. Mild ligamentum flavum thickening should be tolerated well, but severe thickening can cause canal stenosis and foot drop. It is important to note that thickening of the ligamentum flavum is relatively common with spondylolisthesis, and in such instances, even mild thickening may produce a foot drop.
Often, surgeons recommend spinal fusion for patients with spondylolisthesis. In the absence of spondylolisthesis, they may recommend either a discectomy (partial or complete), disc replacement, a foraminotomy, or a combination of both. However, my suggestion is to seek effective conservative care from chiropractors and physiotherapists combined during each therapy session. However, you should avoid any chiropractic or physiotherapy treatment where the spine is “cracked” (rotatory manipulation) or any therapy, exercise, or stretching that puts the spine in flexion, extension, or rotation (twisting) as these can lead to further damage to both joints, discs, and nerves.
If you are experiencing bowel and bladder issues, you may not benefit as much from conservative care as loss of bowel and bladder control is a dangerous stage and in need of immediate surgical intervention.
If you are interested in exploring how our tailored conservative treatments can help alleviate your symptoms and improve your mobility, please don’t hesitate to WhatsApp us at +(60)17-269-1873. We are here to help you recover and regain strength through our comprehensive, integrative care strategies.
Please contact our center to discuss your situation further or to schedule an appointment. You can reach us via our contact details below.
Wishing you the best in health and a swift recovery.
Warm regards,